Q & A: Skin Cancer, Prevention & Dermatopathology
What types of skin lesions or concerns should prompt a referral to a dermatologist for a skin cancer evaluation?
Patients should be referred to a dermatologist for evaluation of any new or changing moles—particularly those with asymmetry, irregular borders, multiple colors, a diameter greater than 6 mm or an evolving appearance (ABCDE criteria). Non-healing sores that bleed, crust or persist for several weeks, as well as rough, scaly patches that may represent actinic keratoses, also warrant referral.
Other concerning features include pearly, translucent bumps or lesions with rolled borders (suggestive of basal cell carcinoma), firm red nodules or scaly growths that may crust or bleed (suggestive of squamous cell carcinoma), and dark streaks under fingernails or pigmented lesions on the palms, soles or mucous membranes—especially in patients of color. Additional referral considerations include any patient with a personal or family history of skin cancer, lesions located in high-risk or cosmetically sensitive areas (such as the face, ears, scalp or genitals), or any lesion that the primary care provider is uncertain about.
Early referral improves outcomes and allows for timely biopsy and dermatopathology review when indicated.
How quickly are patients with suspected skin cancer typically seen after a referral?
Patients with suspected skin cancer are prioritized and can typically be scheduled within one to two weeks of referral. Urgent cases may be expedited based on the clinical presentation or at the request of the referring provider.
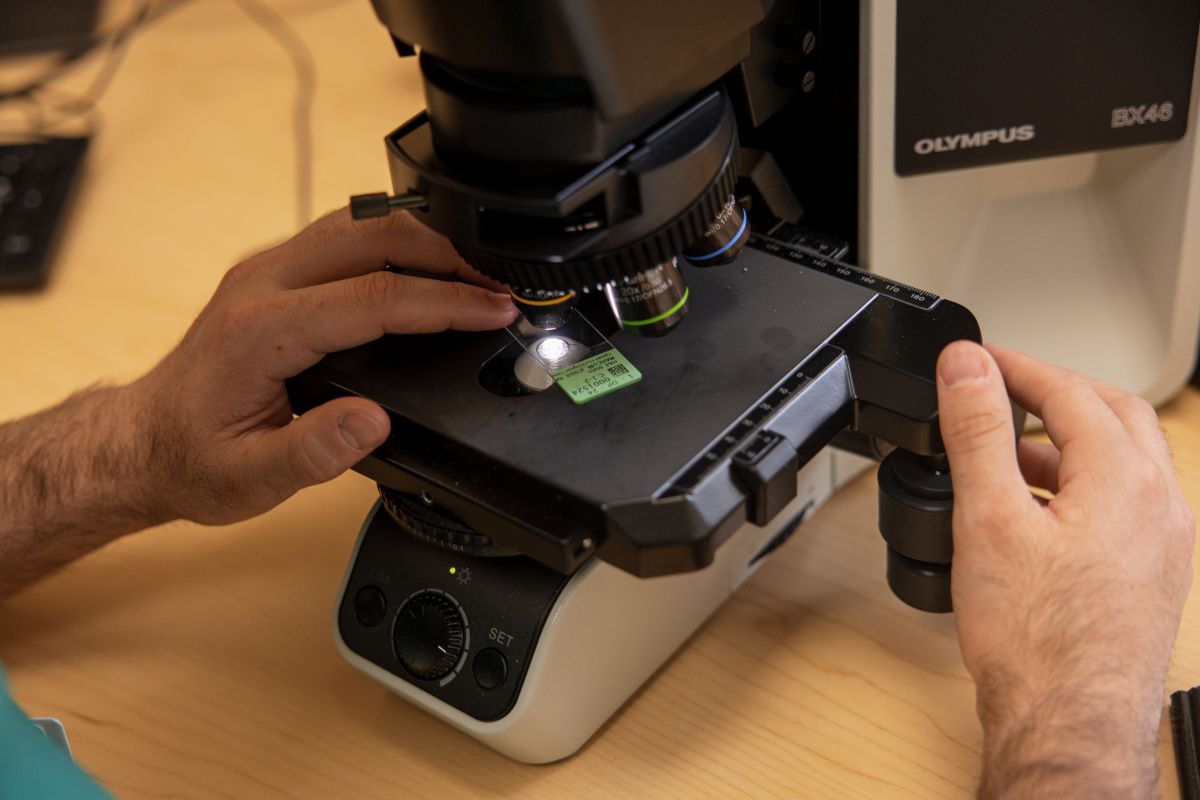
What is the role of dermatopathology in diagnosing skin cancer?
Dermatopathology plays a critical role in diagnosing skin diseases by examining tissue samples under a microscope to identify and classify skin cancers and other conditions. This microscopic analysis helps distinguish between benign and malignant lesions and determines the type and stage of skin cancer, which is essential for appropriate treatment planning.
How are biopsy results communicated back to the referring provider, and what is the typical turnaround time?
Biopsy results at Marshall Dermatology are typically available within three to five business days. For internal referrals, results are shared directly through the Epic electronic medical record system. External providers receive results by fax, and our team may also call directly with urgent or high-priority findings. In complex cases, our dermatologists or dermatopathologist may personally reach out to discuss the pathology report and next steps in care. Our goal is to ensure that referring providers receive timely and accurate information to support continued patient management.
How do you coordinate treatment plans with referring providers once a skin cancer diagnosis is confirmed?
Once a skin cancer diagnosis is confirmed, we notify referring providers within three to five business days of the biopsy. Our dermatologists outline the treatment plan—whether surgical excision, topical therapy or oncology referral—and share it directly with the provider. We prioritize collaboration, especially for patients with comorbidities, and coordinate additional referrals (e.g., Mohs surgery, lymph node evaluation, oncology) as needed. Referring providers are kept informed throughout to ensure seamless, patient-centered care.
What follow-up care or surveillance should referring providers be aware of after initial treatment?
Ongoing surveillance is essential following treatment for skin cancer. Patients should undergo regular skin exams every three to six months for the first one to two years, depending on cancer type and severity, and then annually for long-term follow-up. Primary care providers can help by educating patients on the importance of monthly self-skin checks and prompt reporting of any new or changing lesions. High-risk individuals—including those with a history of melanoma, multiple skin cancers, immunosuppression or significant sun damage—often require dermatology follow-up every six months for at least five years post-treatment. Marshall Dermatology provides continued care for these patients and keeps referring providers informed of surveillance plans and any findings.
Do you offer Mohs surgery or coordinate with specialists for complex or high-risk skin cancers?
The majority of skin cancers can be removed in the outpatient clinic at Marshall Dermatology. However, Marshall Dermatology coordinates care with trusted regional Mohs surgeons for patients who require specialized treatment for complex or high-risk skin cancers. A fellowship-trained Mohs surgeon will join our practice in July 2026, allowing full-time, in-house Mohs micrographic surgery at our Elm Street clinic in Huntington, further enhancing access to specialized care for skin cancer patients.
What is the best way to refer a patient to Marshall Dermatology?
Providers may refer patients to Marshall Dermatology in several ways.
- Internal referrals within Marshall Health Network may be made directly through the electronic medical record by selecting the dermatology referral order.
- Referrals may also be made by calling the main Marshall Dermatology scheduling line at 304.691.1930 or by faxing referral documentation to 304.691.1973.
